Abstract
Introduction: The true incidence of HLH has been challenging to quantify given the diagnostic challenges and overlap with other inflammatory conditions. HLH is characterized by the activation of cytotoxic T-cells and overwhelming cytokine production and release, resulting in extreme inflammation. Primary HLH is most common in children with an inherited genetic mutation. In contrast, acquired HLH refers to patients with an inciting event. Despite the availability of diagnostic criteria, the diagnosis of HLH remains challenging and requires a high-index ofclinical suspicion.
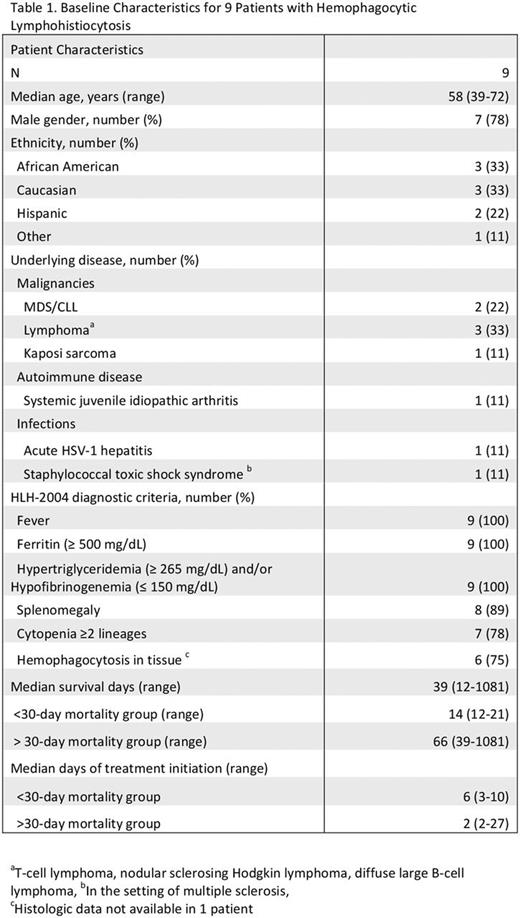
Methods: We conducted a retrospective review to assess the outcomes of HLH cases at our urban institution between January 2010 and June 2017. Data was collected until date of death or last day of data collection. We identified nine patients with HLH. We recorded patient characteristics including underlying condition, criteria for diagnosis, treatment and outcomes at 30 days after diagnosis.
Results: Nine patients were diagnosed with HLH based on the HLH-2004 criteria. Median age was 58 years, and 7 were male. Associated conditions included malignancies (6, 67%), infections (2, 22%), and one patient (11%) with adult systemic juvenile idiopathic arthritis. (Table 1). One patient developed HLH in the setting of Kaposi's sarcoma. All nine patients met at least 5 diagnostic criteria for HLH. All presented with fever and elevated ferritin (≥500µg/L) (median 17,931 µg/L, range 681-40,000 µg/L). Bone marrow examination was performed in 8 patients, six had morphological evidence of HLH (75%). NK-cell level and sIL2R testing were not performed. Seven patients (78%) received etoposide and dexamethasone, two patients (22%) received rituximab in the setting of underlying malignancy, and one received acyclovir and steroids for HSV-1-associated HLH. Four patients died within 30 days from diagnosis (44%), and three patients died after that predetermined time. Two patients were lost to follow-up. Median survival after diagnosis was 39 days (range, 12-1081 days). Patients who died within 30 days of diagnosis had higher ferritin levels compared to the > 30-day mortality group (28,966 µg/L vs. 12,695 µg/L). The median time-to-treatment differed in both groups, 2 days (2-27 days) in the > 30-day survival group, and 6 days (3-10 days) in the < 30-day survival group (Table 1).
Conclusion: Our cohort illustrates the heterogeneity of precipitating conditions for HLH. In our cohort, the median survival was 39 days, reflecting the high mortality associated with HLH. Although small, our results demonstrate a higher mortality in patients with higher ferritin levels, emphasizing the importance of prompt diagnosis and treatment. Despite treatment, the prognosis of HLH remains very poor. Multiple clinical trials are ongoing to help determine the efficacy of novel therapies, including biological agents targeting interleukins involved in the cytokine storm. In addition, ongoing trials will help improve our knowledge of this disease process including genetic information that may reveal an increase in inherited HLH in the adolescent and adult population.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal